Media Release:
Venous leg ulcers are common and distressing, affecting around 1 in 300 adults in the UK. They are open, often painful, sores on the leg that take months to heal and can develop after a minor injury. People with enlarged veins known as varicose veins are at high risk of developing venous leg ulcers, as they have persistently high pressure in the veins leading to skin damage.
In a clinical trial, led by researchers at Imperial College London and clinicians at Imperial College Healthcare NHS Trust, 450 patients with venous leg ulcers were treated with early surgical interventions. This resulted in faster healing and a reduced risk of the condition coming back compared with current methods of treating patients with compression stockings and delayed surgical interventions.
The researchers behind the study, published in JAMA Surgery, suggest that current guidelines on treating leg ulcers should be revised to include early assessment of varicose veins and surgical treatment of leg ulcers to deliver clinical benefits and cost savings for the NHS. They suggest that this early treatment intervention could save the NHS an estimated £100 million per year.
Lead author of the study Professor Alun Davies, Professor of Vascular Surgery at Imperial College London and a Consultant Surgeon at Imperial College Healthcare NHS Trust, said:
“Venous leg ulcers cause enormous physical and mental distress to patients as well as having a financial impact on the NHS. Our study is the first to show that early surgical treatment of leg ulcers leads to faster healing and the reduced risk of the ulcer coming back compared to current methods.
The NHS spends around 2 per cent of its budget on managing lower limb wounds and there is an urgent need to find more effective treatments. We believe that the current guidelines should be changed so that patients with leg ulcers are treated with surgery at an earlier stage. This approach will lead to better outcomes and improve patients’ quality of life.”
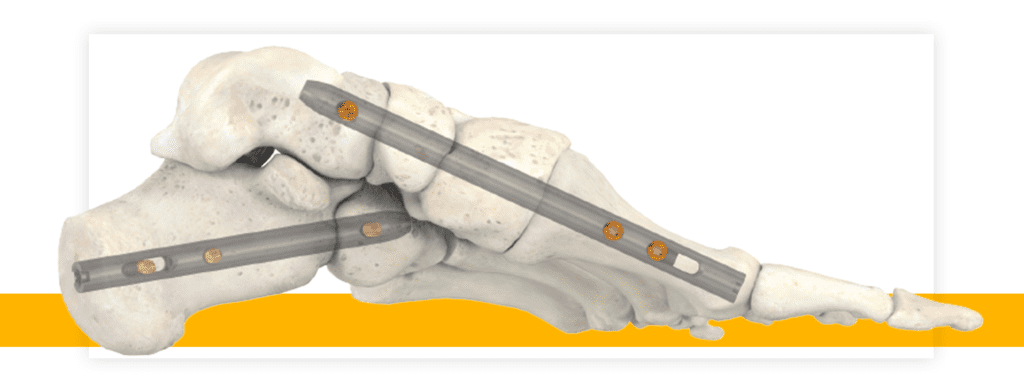
The main treatment for leg ulcers is compression bandages or stockings, to improve the vein function in the legs. There are also surgical treatments such as endovenous ablation – a ‘keyhole’ treatment to close varicose veins. The treatment, under local or general anaesthetic, involves a small fibre passed through a catheter and positioned at the top of the varicose vein. The fibre delivers bursts of energy that heat up the vein and seal it closed. However, under current guidelines this treatment is not usually offered until the ulcer has been present for many months, if at all. Furthermore, if the underlying cause of the ulcer is not treated there’s a high risk of the ulcer coming back after treatment.
The researchers wanted to see whether performing endovenous ablation to treat varicose veins at an earlier stage can lead to faster healing and reduce the risk of venous leg ulcers returning, requiring further treatment.
Researchers recruited 450 patients with venous leg ulcers from October 2013 to September 2016. All patients had leg ulcers of less than six months old and were treated at 20 hospitals in the UK, including Imperial College Healthcare NHS Trust hospitals. Two hundred and twenty four patients were randomly assigned to receive endovenous ablation within two weeks of randomisation followed by wearing compression stockings. The rest of the patients were given compression stockings but the endovenous ablation treatment was delayed by six months or until the ulcer was healed. The researchers then followed up over a period of five years to compare how quickly they healed and the rate of leg ulcer recurrence after treatment.
Of the 426 participants whose leg ulcer had healed, 121 participants experienced at least one recurrence during follow-up. In the early-intervention group, 56 patients experienced recurrence during follow-up. In comparison, 65 participants in the delayed intervention group experience recurrence during follow-up. The rate of recurrent ulcers was 60 per cent higher in the deferred intervention group (0.16 per year of follow-up compared to 0.1 per year in the early-intervention group). They also found that healing was shorter in the early intervention compared to the deferred intervention group.
The team compared the cost of early surgical intervention with delayed intervention over three years and found that early intervention was, on average, the less costly strategy over three years.